Motor Speech Disorder
What is Motor Speech Disorder?
Motor Speech Disorder can take many forms:

Timing and speed of speech

Loss of vocal quality: in pitch, tone and range

A lack of volume and strength

Breath control and steadiness
Motor Speech Disorder – Dysarthria
Speech and swallowing difficulties, caused by oral motor weakness and oral pharyngeal paralysis, have long been reported in the historical literature on polio and post-polio. Although speech and swallowing difficulty are often present in the acute stages of the initial attack, it usually subsided or disappeared after several weeks.
In cases in which bulbar polio was diagnosed, speech and swallowing impairments may have lingered, but most survivors learned to produce compensatory maneuvers to aid them to speak and swallow and did not complain of difficulty.
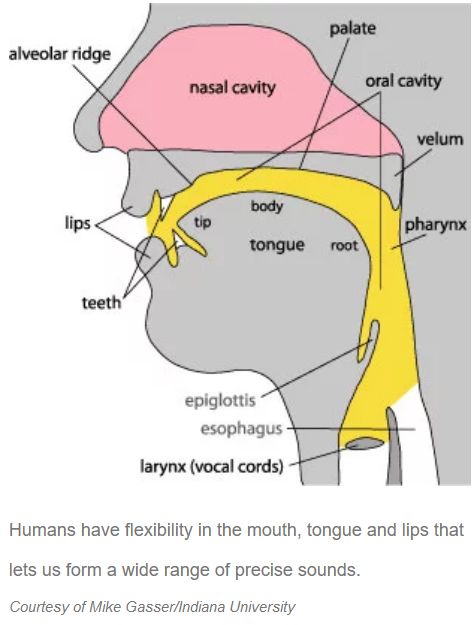
Any motor speech disorder resulting from neurological injury of the motor component of the motor–speech system, such as those caused by Polio, is known as Dysarthria and is characterized by poor articulation of sounds or phonemes.
In other words, it is a condition in which problems effectively occur with the muscles that help produce speech, often making it very difficult to pronounce words. It is unrelated to problems with understanding language (that is, dysphasia or aphasia), although a person can have both. Any of the speech subsystems (respiration, phonation, resonance, prosody, and articulation) can be affected, leading to impairments in intelligibility, audibility, naturalness, and efficiency of vocal communication.
In treating a hoarse voice in people with LEoP, a multidisciplinary team can help maximize and preserve function, considering weakness of the abdominal muscles, diaphragm, and laryngeal muscles.
Dysarthria that has progressed to a total loss of speech is referred to as Anarthria.
Common symptoms of speech disorder include:
A continuous breathy voice
Irregular breakdown of articulation
Monopitch
Distorted vowels
Word flow without pauses
Hypernasality
Changes in speech patterns.
Changes in speech patterns is a comparatively rare, but very real, symptom of the Late Effects of Polio and is thought to be largely confined to those people that had the bulbar form of polio.
On average,within every 100,000 persons infected by the poliovirus, there will be approximately 1000 with paralysis, and of these, about 400 will have clinically persisting paralysis/paresis and about 40 will have the bulba form of poliomyelitis.
Bulbar poliomyelitis results from paralysis of muscle groups innervated by the cranial nerves, especially those of the soft palate and pharynx, which may present as dysphagia, nasal speech, and sometimes dyspnea. The frequency of the bulbar form of the disease has varied in different epidemics from 5% to 35% of paralytic cases.
If you are experiencing changes in speech get an assessment from a speech therapist and explore the options that might be available to you.
What can I do to improve my speech?
Here are some key principles:
Speak slowly and loudly.
Start with a topic word, so listeners know what you want to talk about.
Avoid talking when you feel tired.
Use shorter sentences and pause frequently.
Check to make sure your listeners understand.
Write or draw if you’re having difficulty talking.
Learn sign language – it’s fun, good for the brain and can give you other options for communication while saving your voice.
Social Effects of Dysarthria
Speech difficulties interfere with our relationships and ability to communicate, a fundamental human need, so the social effects are built into the condition. In many interactions, people with dysarthria cannot be fully understood, which makes it difficult and frustrating to engage in daily tasks and can lead to feelings of isolation and loneliness.
Your family, friends and loved ones can use these strategies to improve communication with you. They should:
- Talk to you in a quiet area with good lighting
- Pay close attention to you when you’re talking
- Let you know if they don’t understand what you’re saying
- Repeat what they did understand, so you don’t have to start from the beginning
- Ask yes or no questions to help you communicate
- Encourage you to write or point if you’re having trouble
How is dysarthria diagnosed?
Your healthcare provider will ask you about your medical history and do a physical exam. A speech-language specialist may also evaluate you to help figure out how severe the problem is. They will check your ability to breathe and move your lips, tongue and face. You may need to do some movement and language tasks, such as:
- Bite your lower lip
- Blow out a candle
- Count
- Repeat words and sentences
- Sing
- Stick out your tongue
What tests might I need to diagnose dysarthria?
Other tests you may need include:
- MRI or CT scans of the neck and brain
- Evaluation of your ability to swallow
- Electromyography to test the electrical function of your muscles and nerves
- Blood tests (to look for signs of infection or inflammation)

How is dysarthria treated?
Your healthcare provider will create a treatment plan for you based on the severity of your symptoms. People with dysarthric speech benefit from speech therapy to improve communication. Speech-language pathologists can also work with your family and loved ones to help them learn how to better communicate with you.
During speech therapy sessions, you can learn:
- Exercises to strengthen mouth muscles
- Ways to slow down speech
- Strategies to speak louder, such as using more breath
- Ways to say sounds clearly
- Movements to chew and swallow safely
- Different communication techniques, such as gestures or writing
If the condition is severe, you may need a device to communicate with people. These devices include a letter or picture board or a special computer with a keyboard and message display.
Find out more
Resources, Links and Research Downloads
The Role of Exercise in Post Polio Syndrome: Limbs, Speech and Swallowing
Q: The long term consequences for polio survivors of the epidemic of the late 1940″s and 50’s, is now termed “post polio syndrome” and late effect symptoms” may include: weakness of the limbs, muscle fatigue or pain. Bulbar symptoms may include: new problems with breathing, swallowing or speech. Current evidence suggests that exercises are often beneficial provided that the exercise program is designed for the individual following a thorough assessment and is supervised initially by knowledgeable health professionals.
Who: Joan Headley, executive director of Post-Polio Health International (PHI)., and editor: Ventilator-Assisted Living,
Who: Dr Barbara Sonies, Board Certified Specialist Swallowing, and former Chief of Speech Language Pathology Section and Oral Motor Function Section, Department of Rehabilitation Medicine at NIH, has conducted research and published on neurologic, neuromotor and systemic conditions that impact on swallowing function.
Pharyngolaryngeal manifestations of post-polio syndrome
Q: Review the clinical characteristics and pathophysiological of PPS,as well as present the approach in cases with pharyngolaryngeal manifestations.
W: We present the clinical case of a male patient 48 years old, with main complaints of dysphonia, dysphagia and previous history of polio.
A: The pharyngolaryngeal manifestations of PPS are susceptible to treatment, obtaining satisfactory results, with improvement of life quality of the patients.
