What is Musculoskeletal Weakness?
Musculoskeletal Weakness can take many forms:

Fatigue is often overwhelming, both physical and mental

Loss of muscle strength and/or use also in muscles below the line of clinically evident weakness at the time of the original infection

Loss of muscle endurance

Pain in muscles and joints
Musculoskeletal Weakness
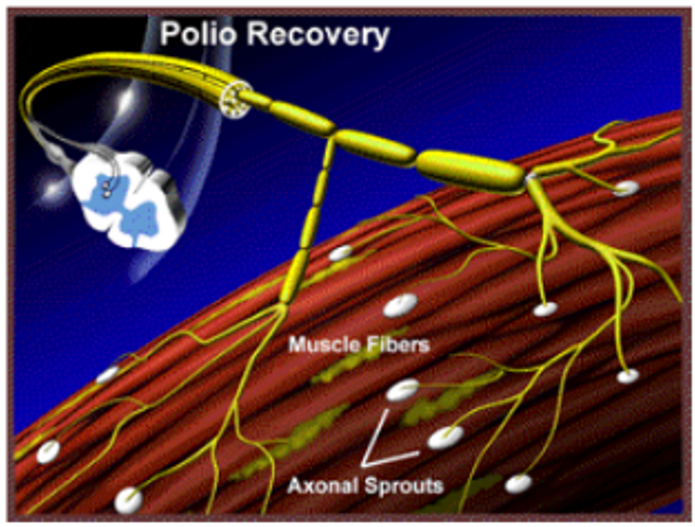
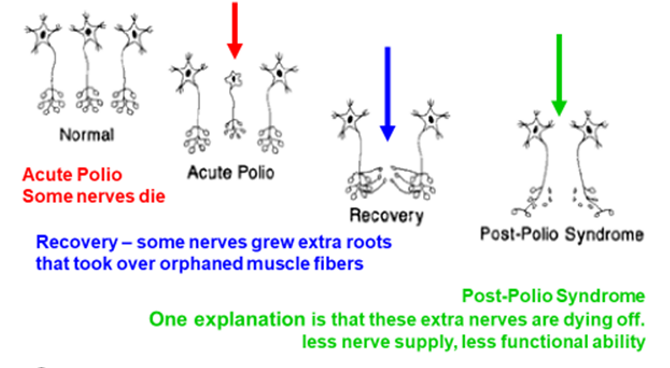
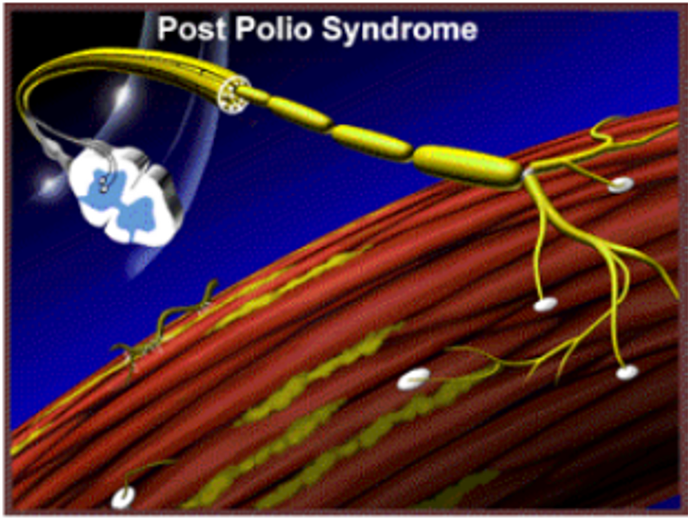
A muscle has a number of nerves supplying it to work.
The poliovirus kills and damages nerves and the resulting ability depends on the numbers remaining.
Recovery was possible because nerves that were not affected grew extra (axonally sprouted) nerve endings that re-innervated some muscle fibres that had lost their nerve supply.
Common symptoms of increasing Musculoskeletal Weakness include:
Progression of deformities in joints
Change in gait
Change in balance and falls
Fatigue increase
Longer recovery times
Changes in Musculoskeletal weakness
In general, muscles stay the same if you treat them the same, and for the able bodied, if you ask them to do more they will develop strength and if they do less they will weaken.
The same applies to people who have had polio, but with a very important caveat. That is, if you do more than your body is capable of doing, you will overuse your muscles and you can suffer long term decline in function, right back to no function at all.
What the level of overuse is will be unique to everybody, as will be the level of maintenance activity. However if you reduce the use of your muscles to virtually nothing in the fear of over using your muscles, the same results might occur.
In general, there are four main reasons why people who had polio may experience musculoskeletal weakness.

What can I do to improve my Musculoskeletal weakness?
Here are some key principles:
Recognize and avoid muscle overuse.
Protect overused muscles.
Recognize deconditioning.
Exercise if appropriate.
Strengthening, aerobic conditioning, and stretching can be beneficial.
Orthosis and/or assistive devices may allow more productive activity and exercise.
Careful pacing and monitoring.
Social Effects of Musculoskeletal Weakness
Musculoskeletal weakness effects our capacity to perform tasks that are essential to living. These range from our mobility, our ability to perform tasks, our ability to work with others, ability to communicate with our bodies and the messages our bodies give, irrespective of our intentions. Also affected others perceptions of us and the stereotypes which may provoke isolating behavior fro others.
This may make some people isolate themselves to protect them from the judgment of others, and in turn effects mood and give rise to feelings of isolation and not belonging. Others go in the opposite direction, maintaining a persona 🙂 to divert attention from their impairments, creating another kind of social distance.
Ongoing worry about Musculoskeletal Weakness
Worry is a perfectly reasonable response to experiencing the body getting weaker and losing our capacity to do things. The future becomes less predictable and the things we find meaning in doing may become harder or impossible to do.
The only antidote to worry is taking action and fighting back. Polio survivors are used to doing that. The thing that is different in this battle is that the enemy is overuse, and the drivers behind that behavior. It is not about blaming ourselves, or others, for why we are wearing out quicker than we have to.
It is about recognising that we have a problem, wanting hard enough to do something about it, finding out what we need to know to be effective, taking the actions needed, with the support of other key people, and then baking it into our life as the best way of living for now.
Impaired Sense Musculoskeletal Weakness
Our impaired sense of musculoskeletal weakness is a learnt ability, allowing us to ignore body signals, keep on functioning at a high level so that we could perform our expected functions. Many of us maintained this well into maturity until the signals managed to become noticeable, even to us.
Unlearning a lifetimes conditioning is no easy thing, yet it is the skill the we need the most to stop progressive weakening. We have to focus on understanding and listening to our body, taking notice of what we perceive, and acting in a way we know is in our best long term interest. It helps if we have help.
Monitoring Your Musculoskeletal Weakness
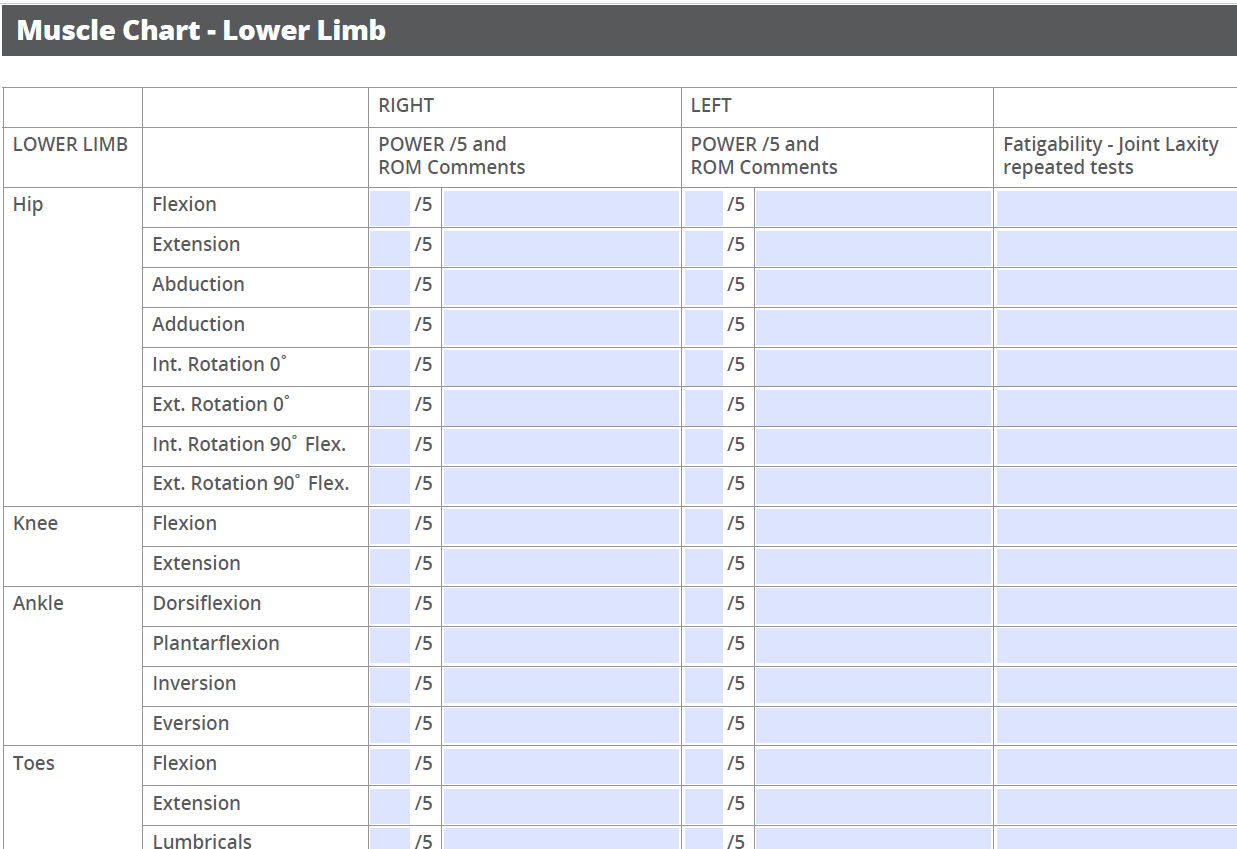
Gaining accurate baseline information for strength, flexibility and joint stability is important to enable appropriate planning for exercise programmes and for establishing what other interventions may be required. It is also useful in conjunction with a thorough gait analysis as muscle testing can help explain gait patterns
Strength
Monitoring our musculoskeletal weakness require measuring the strength and endurance of our muscles and the range of motion of our joints.
Consistency with the testing procedure is critical. For example, changing where the application of force is applied affects the length of the lever arm and therefore the muscle torque – shorter lever arms will provide higher testing scores when compared to using longer lever arms.
The test should be completed on the uninvolved or stronger side first to determine what normal strength is before being repeated on the involved side.
Strength is recorded through full active range and also isometric resistance at mid-range.
If full range is not achieved eg only gains ¾ range in a good movement pattern, then the strength is marked down because of not reaching full range.
Oxford scale
Oxford scale is used.
0 – No contraction present
1 – Flicker contraction
2 – Full ROM, gravity eliminated
3 – Full ROM against gravity
4 – Full ROM against gravity + added resistance
5 – Muscle function normal
Grade 3, movement against gravity, is a good guide to indicate if recovery is achievable as generally Grade 3 and above can be strengthened but Grade 2+ and below are unlikely to get higher.
Scoliosis
The shoulder and scapular movement needs to be observed as kypho-scoliosis impacts on shoulder movement.
All trunk movement is tested – flexion, extension, side flexion (fingertip to lateral knee) and rotation in unsupported sitting.
Bending down to pick up an object from the floor can be used as a test and can highlight compensatory movements.
Range of Movement
Usual orthopeadic range of movement (ROM) scale is used for passive and active ranges.
Active and passive ROM recorded for all limbs, neck and spine.
Limitations in expected range could be due to weakness, contractures or deformity and both active and passive ROM should be assessed.
Find out more
Resources, Links and Research Downloads
Duncan Foundation Muscle Assessment Form
Q: Duncan Foundation Assessment Form
W: Documents accurate baseline information for strength, flexibility and joint stability
A: Register with the Duncan Foundation to get a proper assessment here.
