What is insomnia?
Insomnia can take many forms:

You may find it hard to fall asleep or stay asleep during the night

You may wake up too early

When you wake up in the morning you don’t feel refreshed

Poor sleep makes it harder for you to function during the day
Insomnia is not defined by the number of hours you sleep, because each person needs a different amount of sleep.
In some people, insomnia may be linked to other medical conditions, such as sleep apnoea, depression, stress, and pain. Poor sleep can lead to heart disease, diabetes and stroke. The fact is that sleep problems are important and should not be ignored.
Common symptoms of insomnia include:
Difficulty falling asleep or staying asleep
Variable sleep, such as several nights of poor sleep followed by one night of better sleep
Daytime fatigue or sleepiness
Forgetfulness
Poor concentration
Irritability
Anxiety
Depression
Reduced motivation or energy
Increased errors or accidents
Changes in Sleep Patterns
Many older people notice is a change in their sleeping patterns, be it harder getting to sleep, sleeping less, having interrupted sleep, restless leg, cramps, or they just feel less rested when they wake up.
The number of times a person wakes up after they’ve fallen asleep, the amount of time someone spends in the lighter stages of the sleep cycle (so called “Stage 1” and “Stage 2” sleep), and the total amount of time a person spends asleep are all factors which change as a person gets older. Aging people increasingly wake up during the night, spend more time in lighter sleep stages and spend less time in deeper sleep stages, and spend less total time asleep.
In general, there are four reasons why people who had polio may have trouble sleeping.

What can I do to improve my insomnia?
Here are some key principles:
Sleep only long enough to feel rested and then get out of bed.
Go to bed and get up at the same time each day.
Avoid forcing sleep.
Exercise regularly (low-impact, interval training) but not 4 to 5 hours before you go to bed.
Social Effects of Insomnia
For many people, insomnia affects their relationships, job performance, and daily function. In one survey, people who had chronic insomnia were twice as likely to have a car accident compared to people who were tired for other reasons.
Ongoing worry about sleep
One result of poor sleep is that you may worry that you will be sleep-deprived and will suffer from serious consequences of lost sleep. This concern may grow as you are unable to sleep, which in turn makes it increasingly difficult to fall asleep. It is important that you not get caught in this cycle and understand that you are sleeping more than it seems.
Impaired Sense of Sleep
People with insomnia have an impaired sense of sleep. You may feel that you have not slept, even if testing shows that you have. You may also feel more tired and worn out than people who don’t have insomnia, even if testing shows that you are less sleepy. This impaired sense of sleep may be related to a problem with the body’s sleep arousal system, which normally helps you feel awake after sleeping and feel tired before going to bed.
Monitoring Your Sleep
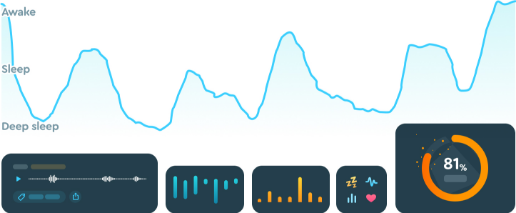
A wide variety of sleep trackers have hit the market, with more being released all the time. Many are wearable trackers that you can strap to your wrist. Others clip on your pillow or sit on your bedside table. Features of these devices vary, but some common capabilities include:
Sleep duration: By tracking the time you’re inactive, the devices can record when you fall asleep at night and when you stir in the morning.
Sleep quality: Trackers can detect interrupted sleep, letting you know when you’re tossing and turning or waking during the night.
Sleep phases: Some tracking systems track the phases of your sleep and time your alarm to go off during a period when you’re sleeping less deeply. In theory, that makes it easier for you to rouse.
Environmental factors: Some devices record environmental factors like the amount of light or temperature in your bedroom.
Lifestyle factors: Some trackers prompt you to enter information about activities that can affect sleep, such as how much caffeine you’ve had, when you’ve eaten or whether your stress level is high.
Recognizing Sleep Patterns
While sleep trackers can collect a lot of information about your slumber habits, there’s one important thing they generally don’t do, says Alan Schwartz, M.D., director of the Sleep Disorders Centre at Johns Hopkins Bayview Medical Centre: “They don’t measure sleep directly,” he says.
Instead, they often measure inactivity as a surrogate for estimating sleep, he explains. “Most sleep tracking devices make some guesstimate as to how much you’re actually sleeping.”
For exact data about your sleep habits, you’d have to do a medical sleep study, which monitors brain waves to analyse the stages of sleep you cycle through during the night. Such studies are helpful for diagnosing conditions like sleep apnoea and other sleep disorders.
Still, tracking devices can be useful for helping you recognize patterns in your sleep habits, Schwartz says. Do you feel sluggish when you sleep from 10 p.m. to 6 a.m. but energetic if you shift your shuteye to 11 p.m. to 7 a.m.? Do you sleep better when your bedroom is cooler or on days you exercise? Is your sleep disrupted if you have caffeine after lunchtime?
“The tracker will give you something to reflect on,” says Schwartz – often with user-friendly graphs or reports that make it easy to spot trends. If you have any concerns about the quality of your sleep, it’s a good idea to talk to a doctor.
If you’re an otherwise healthy person who just wants to gain some insight into your sleep routine , tracking devices might be a good option. “Just take the numbers with a grain of salt,” Schwartz says.
Find out more
Resources, Links and Research Downloads
Video link to Andrew Veal Sleep
Q: Andrew Veal is a sleep clinician who has worked throughout his career with people living with the late effects of polio.
W: A recording of his presentation on sleep to the Polio NZ AGM Hamilton 2013
A: All you ever wanted to know about the Late Effects of polio and Sleep.
Analysis of sleep characteristics in post-polio syndrome patients
Q: To analyze sleep patterns in PPS patients
W: Sixty polio survivors complaining of sleep disturbances were evaluated by means of polysomnography, performed at the Sleep Institute
A: New post-polio sleep disturbances were isolated symptoms. It appears that these symptoms were not due to post-polio features, but rather, that they were due to dysfunction of the surviving motor neurons in the brainstem. Abnormal dopamine production, which is responsible for many sleep-related breathing disorders and abnormal movements, may also have been implicated in the present findings.
