What is Pain?
Pain can take many forms:

Post-Polio Muscle Pain: This is the pain people experience in the muscle tissue itself

Overuse syndromes and soft tissue pain: Caused by injury or inflammation of soft tissues: muscles, tendons, bursa, and ligaments

Biomechanical/degenerative disease pain: Changes in normal joints due to wear and tear

Bone pain: can be very severe pain; it can be kind of a deep ache
What is pain?
This may seem like a silly question, as everyone has experienced pain at some point in his or her life, whether short and sharp or a long lasting ache. But not everybody understands how and why pain happens. Pain is usually the body’s way of telling us that something is wrong. Most of the pain we experience is caused by actual or threatened damage to the tissues in our bodies, such as muscle and bone.
Most of the tissues and organs of our bodies are served by a network of sensing nerves. These are different nerves to the ones that aid muscle movement – the motor neurons – that can be damaged or destroyed by the Polio virus. The sensing nerves pick up information about any damage, or threat of damage. Chemicals are released, which excite nearby nerve fibres.
Messages about the damage are then carried to the brain via the spinal cord. In specialised areas of the brain, the messages are interpreted as pain coming from the area affected by the damage.
Healthcare professionals use different terms for different types of pain. Short-term pain, such as that from a punch, is called acute, long-term continuous pain is called chronic and pain that comes and goes is called recurrent. Pain can be a very helpful warning sign that damage within the body has started to occur, eg joints becoming irritated.
Pain Management
Pain has the potential to make dramatic changes to someone’s life – affecting both their physical and emotional well being and their ability to remain active and independent.
Pain management is not about curing pain – it is a realistic approach to living with pain and creating a better quality of life for yourself.
No two people who had Polio or have LEoP are going to have the same experience of pain and each will cope with it in his/her own way. Different methods of pain management work for different people. It is important to find which work best for you.
When dealing with pain, there are no easy answers or quick-fix solutions. Painkillers alone can only go so far to control pain.The long-term management of pain is about applying a range of treatments and techniques to help you handle it better and reduce its effect on your life.
With successful pain management, people who had Polio or have PPS are able to get on with living as full a life as possible.
Why do people with Polio or LEoP experience pain?
In people who had Polio or have LEoP, pain may be caused by a number of factors. These include the overuse of weak muscles and the strain on joints, limbs and other parts of the body caused by weakness, paralysis, abnormal posture, gait and body, movements (particularly when substituting for weak muscles) and the long-term use of crutches, callipers and manual wheelchairs.
This pain may be acute, chronic or recurrent, depending upon the cause and some people may experience one or more of these.
People who had Polio or have PPS describe their pain in many ways, including dull aches and/or sensations of throbbing, cramping, burning, twitching, shooting, stabbing, pins and needles and stinging.
Other health conditions that can cause pain
Many people who had Polio or have PPS have fibromyalgia (pain in the fibrous tissues of the body), which is usually described as throbbing, burning or twitching sensations. Osteoporosis is also common and this can cause painful fractures.
Rheumatoid arthritis or osteoarthritis are also frequently a problem for people who had Polio or have PPS. Arthritis pain can be caused by the inflammation of joints, which can cause swelling and loss of movement.
Post Polio muscle pain
Post Polio muscle pain occurs in muscles affected by the original Polio illness and is described as either a deep or a superficial aching pain. People may also experience cramping and fasciculations, often described as a crawling sensation. This type of pain often occurs at night-time or the end of the day and is worsened by physical activity, stress and cold temperatures. It usually decreases or disappears with rest.
This type of pain may be useful in that it can help patients begin to recognise PPS symptoms and also when they may be overdoing activities, in order to apply energy management techniques (see Pacing and energy conservation).

Overuse pain.
This type of pain includes injuries to soft tissue, muscles, tendons, bursa (small fluid-filled sacs that help to reduce friction, such as around joints) and ligaments. A common example is tendonitis from overuse of the shoulders. People who had Polio usually have more leg than arm muscle weakness and will use their relatively stronger upper body to compensate for their relatively weaker lower one, for movements such as getting up from a chair, climbing out of the bath or walking with crutches.

Biomechanical pain
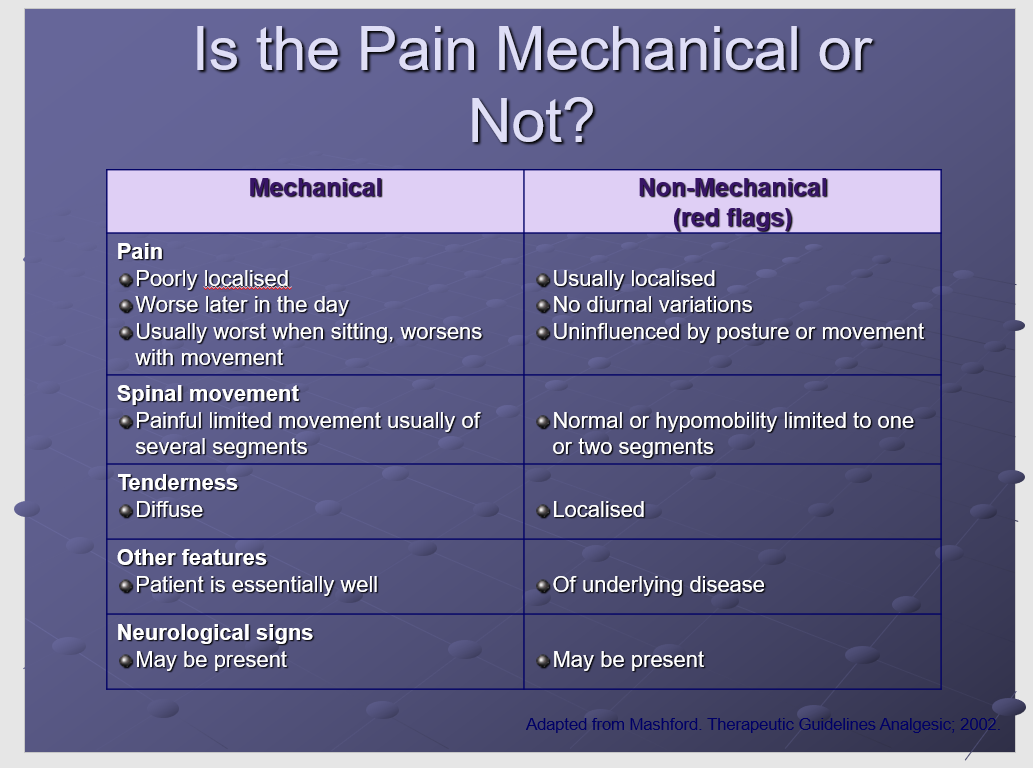
Biomechanical pain occurs as a degenerative joint disease (DJD), lower back pain (particularly when hip muscles are weak or there is scoliosis – curvature of the spine) or pain from nerve compression syndromes, such as carpal-tunnel syndrome.
Weakness brought about by Polio-affected muscles, as well as poor body mechanics, makes the joints more susceptible to the development of DJD. Years of walking on unstable joints and supporting tissue increase the chance of developing further pain and deformity. Those who use manual wheelchairs or devices such as callipers, walking sticks and crutches are prone to DJD, or overuse syndromes in their upper extremities, especially the wrists (ie carpal-tunnel syndrome) and shoulders.

Back pain
People who had Polio may have skeletal abnormalities, such as scoliosis, which put strain on the spinal bones (vertebrae) and supporting muscles, tendons, ligaments and tissues supported by the spine, resulting in pain.
A common cause of lower back pain in people who had Polio is sacroiliac dysfunction. The sacroiliac (SI) joints are on each side of the lower back, at the top of the buttocks. They connect the base of the spine (sacrum) with the hips/pelvis (ilium). Sacroiliac pain is caused by too much movement (hypermobility or instability) or too little movement (hypomobility or fixation). It is usually described as sharp and stabbing or a dull ache and can be worsened by twisting, sitting for long periods or standing with a sway back. Legs of unequal length, an imbalance of muscle in the legs, poor trunk and abdominal muscle control, weight gain, scoliosis, abnormal gait, poor postural habits and trauma or injury from a fall can all cause sacroiliac joint dysfunction.
There are of course many possible causes for back pain and not all of these are directly related to Polio or the health of the back. Some causes are more serious than others, but it is always a good idea to consult your GP, particularly if the pain is new.

Ten useful tips for helping you manage pain
Accept that the pain is there, your pain is part of your life, but it is not you. Don’t fight against it but work with it
Be positive every day and make time for fun and laughter
Seek help and support, don’t suffer in silence; talk about how you are feeling
Pace your activities to prevent further pain – know when to stop
Do things that make you happy and keep your mind active
Learn to relax and make sure you do this every day, socialising, a hobby or interest, learning something new, for instance
Join a pain management course or support group
Look after your general health – eat a healthy diet, make sure you get enough sleep and maintain a healthy weight
Keep a diary to record your progress and learn from experiences that didn’t work for you and note the successes you have achieved
Keep an open mind and be willing to try new ways of helping yourself
The Pain Cycle
Fatigue is already a problem for many people who had Polio or have the LEoP and pain can often worsen this. People can become caught up in a cycle of pain, fatigue, negative thinking, depression and stress, which can make the pain seem worse and therefore much more difficult to deal with. Learning to manage pain can help to break this cycle.
The Pain Barrier.
It is thought that many methods of pain control help to reduce pain by directly closing or blocking what is known as the pain barrier. Pain signals travel to the brain along the spinal cord. The pain barrier is a way of describing whether these signals are allowed to travel to the brain, or are prevented from reaching it.
Closing or blocking this “barrier” in the spinal cord can prevent the signals from reaching the brain, where they are recognised as pain. Both physical and psychological factors are at work here.
If the brain is occupied with other things, the effect of the pain signal can be reduced and you feel less pain. An example of how the pain barrier works is when a mother who is so caught up in the aftermath of her child being injured, does not notice that she has been stung by a wasp just before the accident (this is a true story!) Once she knows her child is going to be okay, the pain “breaks through” the pain barrier and she notices that she has been stung.
The brain and spinal cord can release their own natural painkillers- known as endorphins – that can close the pain barrier naturally. There are various methods of stimulating nerves to release endorphins and block pain. These include massage, heat and physiotherapy. Pleasurable pursuits and positive thinking also have a significant effect in reducing the amount of pain you feel and helping you to respond to it in a more positive way.
Quotes and saying about pain – there is at least two sides to everything.
What can I do to improve my pain?
Here are some key principles:
Post-polio muscle pain: learn to know your limits, how they are changing, and LISTEN to your body.
Overuse pain: change body mechanics, alleviate excess stress, protect affected areas, rest, ice, anti- inflammatory medication, injections, and surgery.
Biomechanical pain/joint: protect or strengthen joints, regain range of motion, unweight, bracing or assistive devices, surgery in select cases.
Biomechanical spine pain: exact diagnosis, modify body mechanics/position, injections, orthotics, surgery if appropriate.

Getting to know your pain.
You may think that this is a rather strange idea. Really getting to know your pain, however difficult this may be, can help to remind you that it is not you, but something separate from you, with its own characteristics, which ebb and flow during the day.
You might like to try keeping a detailed “pain diary” for a few days. Be creative: give your pain a colour, a form; describe it in words. Note the things that make it worse, or that reduce it. Do you notice any patterns emerging? When you have done any of these exercises, consider how your thoughts about your pain have changed.
Medication
Painkilling drugs can make a dramatic improvement to the quality of life of many people living with chronic pain. A reduction in pain can improve sleep and therefore fatigue levels and your ability to function on a day-to-day basis. This can have a very positive effect on your physical and emotional well being, as well as your general quality of life and personal relationships.
Even if taking medication is not your first approach to pain relief, it is useful to know what the options are. You may wish to talk to your GP about what is available.
Some people may be reluctant to take painkillers. This may be because of concerns about side effects. All drugs unfortunately have potential side effects and you may have to weigh up the possibility of these against the obvious benefits of reduced pain. Some people may worry about becoming dependent upon painkillers. If you have any concerns, talk them through with your GP.
You should always seek medical advice before taking painkilling drugs and always inform your doctor and pharmacist of all the medication you are taking.
Further information about painkillers is contained in our factsheet, What you should know about your medication – a guide for people with Polio or Post Polio Syndrome (PPS).
Further information on the risks of self medication can be found here

Physical therapies
Exercise
Taking regular exercise can help you manage your pain. It may be tempting to avoid exercise altogether, for fear of injuring yourself and making the pain worse, but keeping moving will maintain fitness and help your body cope with pain better. Exercise can also release endorphins and increase self-esteem and well being, which also help minimise the impact of pain.
As with pacing, exercise needs to be tailored to the individual, so you are advised to seek help from a registered physiotherapist.
Varying your activities will ensure that you stick to an exercise regime. Little and often is key. Build up slowly and regularly over a few weeks, remembering to warm up and cool down.
Gentle stretching exercises such as yoga or Pilates can help maintain flexibility, while non-fatiguing aerobic exercise can improve the stamina of the heart and lungs, improve blood circulation, lower blood pressure and aid relaxation and sleep – all of which will improve pain management.
Physiotherapy
Physiotherapists can offer a tailored programme to help patients manage chronic pain. This may include specialist exercises, posture management and hydrotherapy.
Hydrotherapy
Hydrotherapy is the use of water to treat a variety of conditions, such as arthritis or back pain. Doing special exercises in a warm- water pool, usually within a hospital physiotherapy department, allows muscles to relax, eases pain and increases the range of movement of joints and can help improve muscle strength.
A physiotherapist will decide if you would benefit from hydrotherapy. You do not have to be able to swim to have hydrotherapy and a physiotherapist will always be in the pool with you.
TENS
Some people who had Polio or have LEoP find TENS machines helpful as part of a pain management programme. TENS stands for Transcutaneous Electrical Nerve Stimulation. TENS machines deliver small electrical pulses to the body via electrodes placed on the skin. It is thought that pulses from the TENS machine “block” pain signals from the source of the pain to the brain. If the brain receives fewer signals, we may then feel less pain.
Relaxation
Muscle tension and stress and anxiety can worsen pain, so learning to relax is a very important part of the pain management process.
Relaxing pursuits, such as listening to soothing music, light reading and gardening can be helpful. You may also wish to try relaxation exercises, guided relaxation CDs, deep breathing or meditation. Try and make time for relaxation every day.
Talking therapies
According to a survey carried out by the British Pain Society, 49% of people with chronic pain become depressed. Talking therapies can help people come to terms with their pain and explore the way it is affecting them and their daily life.
Talking to a counselor, psychotherapist or psychologist allows people to work through their feelings about their pain and to find ways of making changes to help them cope with it better.
Cognitive behavioural therapy
Cognitive behavioural therapy (CBT) is a talking therapy that was originally developed to help treat depression, but the techniques it uses have been found to be highly effective for treating a range of problems.
The basic idea behind CBT is that the ways we think, feel and behave are very closely linked. Changing the way we think about ourselves, our experiences and the world around us, changes the way we feel and what we can do.
During CBT, the therapist helps the person to identify and challenge their negative thoughts, which can help them escape the cycle of negative thoughts and feelings. The therapist also shows the person different ways to cope with unhelpful thinking and behaviour patterns.
CBT has been found to be very helpful for people living with chronic pain, particularly where anxiety appears to be a strong component e.g., the person frequently seeks reassurance, worries persistently and avoids specific movements or situations.
There is an increasing range of pain management self-help manuals available, many of which use CBT principles and techniques. While these can certainly be very helpful, they are no substitute for a suitably qualified therapist.
Pain management programmes
Pain management programmes often involve working in a group with other people experiencing chronic pain. Programme lengths and numbers of sessions will vary. A typical pain management programme is rather like a part- time course, helping people learn more about pain and offering practical strategies and coping skills.
Many people with chronic pain have found these programmes very helpful, particularly as they can receive support from others going through similar experiences and learn about others’ coping methods.
Find out more
Resources, Links and Research Downloads
Previous acute polio and post-polio syndrome: recognizing the psychophysiology for the establishment of rehabilitation programs
Q: A letter from 7 Brazilian LEoP professors on exercise and pain.
W: The purpose of this letter to the Editor is to alert readers about the risks of therapeutic exercise for this people living with the late effects of polio.
A: Physical activity is considered as an adjunct to a good health condition and psychological benefits, provided that it respects the particularities of patients and especially the pathophysiological framework of the Late Effects of Polio.
POST-POLIO PAIN: CAUSES AND MANAGEMENT
Q: The changes, for people living with the late effects of polio, in muscle and body mechanics and the pain syndromes that are the result of that.
W: Overview of the causes and treatment of pain for LEoP
A: It’s your body, your ultimate decision about what you’re going to do or not do. You are responsible for your health. You are the primary person responsible, but find a good health professional who will help you and work with you.
